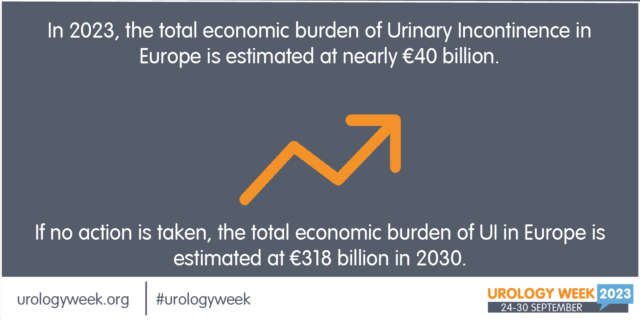
Press release: Incontinence costs European society over 40 million Euros per year
Brussels, 23 September 2023 – New international research on the economic burden of urinary incontinence reveals that the cost of continence care will cost over 40 billionRead more